The Sports Car Collector’s GPT
June 24, 2025The “Big, Beautiful Bill” and the Slow Disembowelment of the American Citizen
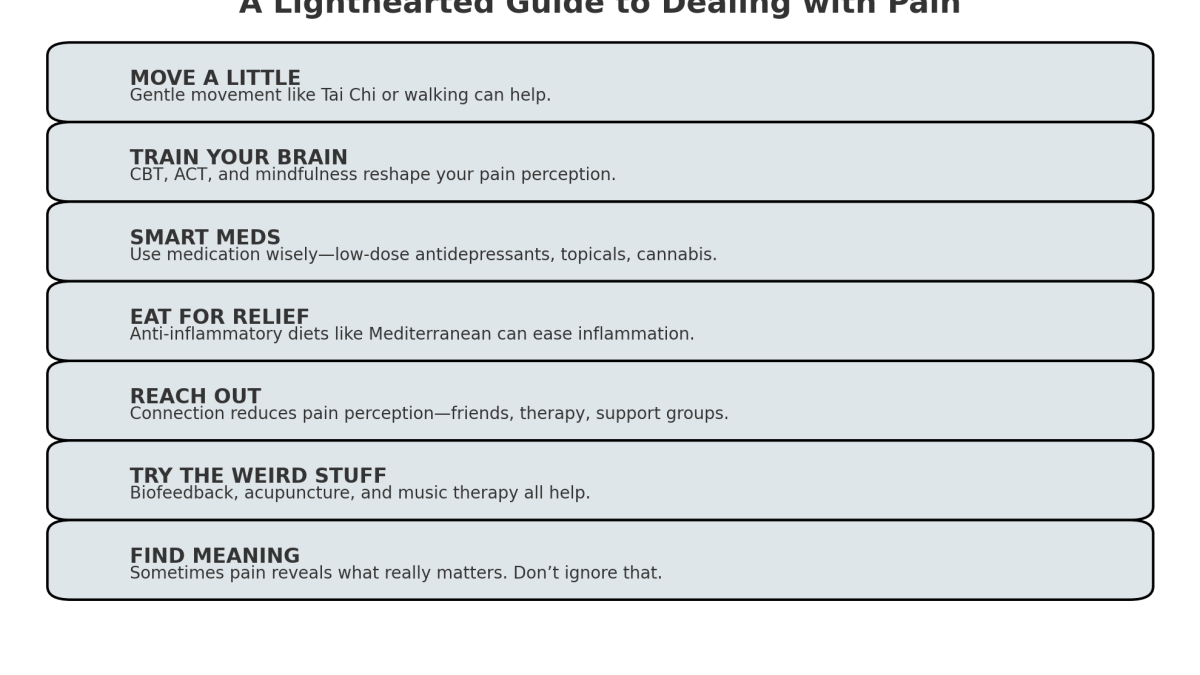
July 1, 2025Let me be honest: I’m no stranger to pain. I carry it in my back, in my joints, in my nervous system (thanks, central sensitization), and sometimes in that odd corner of my chest where heartbreak, failure, and existential dread all like to gather for coffee. Pain has been a constant, sometimes shouting, sometimes whispering, but always there—like a really annoying roommate who never pays rent.
What follows isn’t a miracle cure. If there were one, I’d already have bought it, photographed it, and written a five-part blog series about it. But what I can offer is a collection of the most well-supported, scientifically-backed, and lived-experience-approved methods for managing both physical and emotional pain. Think of it as a care package—less Vicodin, more vitamin soul.
1. Movement (Yes, Even When It Hurts)
“Motion is lotion.” – Every good physical therapist ever
You don’t need to become a triathlete (God forbid), but movement does matter. Studies repeatedly show that gentle, consistent exercise reduces inflammation, boosts endorphins (natural painkillers), and slows the muscle breakdown that can worsen pain.
Evidence-based winners:
- Tai Chi – Shown to improve chronic pain, particularly in fibromyalgia and arthritis. It’s like dance, but slower, with fewer leotards.
- Yoga/stretching – Even light, modified yoga reduces stress and stiffness. And if you’re like me—6’1″, 270 lbs, and slightly creaky—you can do it in a chair and still benefit.
- Walking – Seriously. Start with five minutes. Build from there. Just avoid potholes and rogue chihuahuas.
2. Mind Over Monkey Brain: CBT and Beyond
Cognitive Behavioral Therapy (CBT) has an enormous evidence base when it comes to managing chronic pain and its sneaky partner-in-crime: depression. It doesn’t mean the pain isn’t real—it just means your interpretation of the pain is up for a makeover.
Other effective brain tools:
- ACT (Acceptance and Commitment Therapy) – A cousin of CBT that focuses on living with pain, not fighting it.
- Mindfulness Meditation – Multiple studies show it helps reduce perceived pain by calming the limbic system (our panic center) and retraining the brain’s relationship with discomfort.
- Guided Imagery – Turns out imagining yourself floating in a warm lagoon with dolphins really can reduce cortisol levels. Who knew?
Pro tip: You can use apps like Insight Timer, Headspace, or Curable (which is pain-specific and excellent) to dip your toe into this mind-body toolkit.
3. Medication (But with Eyes Wide Open)
Yes, sometimes we need medication. And there’s no shame in that. The problem is, pain meds—especially opioids—can be a double-edged sword. Many of us have been burned chasing relief and ending up more miserable.
Things that do help, with research to back them:
- Low-dose antidepressants (like amitriptyline or duloxetine) for nerve-related pain
- Anti-seizure meds (gabapentin, pregabalin) also used for fibromyalgia and neuropathy
- Topical treatments – Capsaicin cream and lidocaine patches have surprisingly strong results with fewer side effects
- Medical cannabis – Anecdotally helpful, and increasingly backed by research, especially for neuropathic pain—though legality varies and side effects need to be respected
4. Food Isn’t Just Fuel—It’s Chemistry
No, a kale smoothie won’t heal your broken spine or your broken heart. But chronic inflammation is real, and a Mediterranean-style diet—rich in omega-3s, greens, berries, nuts, and whole grains—has been shown to reduce markers of inflammation and, consequently, pain levels.
And let’s not forget hydration. Dehydrated muscles cramp. Dehydrated brains get cranky. Drink water. It’s free and socially acceptable.
5. Connection: The Most Underrated Medicine
Isolation amplifies pain. It turns up the volume on suffering like a bad sound engineer at an open mic night.
Numerous studies, including some out of Harvard and Stanford, show that connection—especially emotionally safe, empathetic connection—literally changes how our brains process pain. This could mean:
- Talking with a therapist or coach
- Finding (or starting) a chronic pain support group
- Reaching out to old friends—even the weird ones
- Starting a blog, a YouTube channel, or just sitting in a café and making eye contact like a French existentialist
6. The Weird but True Toolbox
These tools don’t get as much mainstream love, but there’s legit research behind them:
- Biofeedback – Trains you to control physical responses like heart rate and muscle tension. Feels like becoming your own Jedi master.
- Acupuncture – Especially for lower back and osteoarthritis pain. If you’re not needle-phobic, it’s worth a shot.
- Music Therapy – Research out of MIT and other institutions shows that certain music—especially classical or ambient—can measurably reduce the experience of pain and anxiety.
(And if you’re like me, pounding industrial metal at 95 decibels helps too—but maybe that’s just a form of emotional exorcism.)
7. The Existential Angle: Pain as Teacher (Yeah, I Know)
This is the hardest part. And it’s not a cure—but it is a perspective. Pain, especially chronic pain, strips away illusions. It asks us: “Who are you, really, when everything else is on fire?”
In my case, I’ve been forced to reevaluate what I value: meaningful writing, connection with my daughter, philosophical inquiry, and of course, cars that go vroom.
Sometimes pain isn’t something to fix. Sometimes it’s something to witness. And in witnessing, we begin to reclaim a bit of power.
Final Thoughts from the Recliner
Pain can shrink your world. But if you’re stubborn, resourceful, and willing to experiment (safely), you can push back. Maybe even laugh once in a while.
So no, I may not be pain-free—but I’m still writing, still dreaming, still occasionally burning rubber in a 911 Cabriolet. And that, my friends, is victory enough for today.
“Pain is inevitable. Suffering is optional.”
– Haruki Murakami (and every pain management seminar ever)